For Participants
Frequently Asked Questions

Take a look at the most frequently asked questions about clinical trials and what they entail. Can't seem to find the answer you're looking for? Call us at 203-419-4404.
What are clinical trials?
They are research studies conducted according to a plan called a protocol. A protocol describes what types of patients may enter the study, the schedule of tests and procedures, drugs, dosages, and length of study, as well as the anticipated outcomes to be measured. Carefully conducted clinical trials are the mechanism to evaluate the safety and effectiveness of investigational drugs.
There are different types of clinical studies—Phase I to Phase IV. Clinical trials can vary in size from a single site in one country to multi-center trials in multiple countries.
Phase I is where researchers test an investigational drug for the first time in humans by administering it to a small number of healthy people to evaluate its safety, determine a safe dosage range and identify side effects.
Phase II is where the investigational drug is given to a larger number of people who have a particular disease or condition to assess how well the drug works and to further evaluate its safety, as well as to continue Phase I safety assessments in a larger group of volunteers. This is often where a new drug fails or when the drug is discovered not to work as expected, or to have toxic effects or side effects.
Phase III is where several hundred to several thousand people with the appropriate disease or condition participate in multi-center studies, often in more than one country. During this phase, the investigational drug undergoes additional testing to further determine its safety and effectiveness, monitor sides effects and compare it to commonly used treatments.
Phase IV is when a drug already approved by prescription is tested to gather additional information on the benefits, risks, and use, for example in different populations whom the treatment was not previously tested.
Who can participate in a clinical trial?
A participant must be eligible for the study and be able to travel to our sites before they may participate in a clinical trial. Some clinical trials seek volunteers with diseases or conditions to be studied, while others require healthy participants. All clinical trials have eligibility requirements for participants. A specific set of criteria for each study is an important principle of medical research that aids in the development of accurate results.
These criteria are based on things like:
- Age
- Gender
- Type and stage of a disease
- Previous treatment history
- Other medical conditions
The criteria are intended to identify suitable participants and keep them safe. All these factors serve to guarantee that researchers will be able to answer the questions they intend to investigate.
How can I join a study at Chase Medical Research?
Once you find a study that you might be interested in, you can call/text us at 203-419-4404 or email us at research@chasemr.com to speak with one of our specialists on clinical trials. We are knowledgeable of the requirements for participation & can determine if you are a good candidate for the trial.
Although you may not qualify for a particular study, to be considered for future studies in a particular therapeutic area, you can ask to be put in our database for notification about upcoming trials.
Can I continue seeing my primary health care provider while in a clinical trial?
Clinical research trials do not interfere with your relationships with your primary care doctors or specialists, and you should maintain your relationships with your doctors. It is important that your own doctors communicate any treatment or changes in your health status to the clinical trial site staff while you are participating in the trial. By collaborating with the study team, the participant can ensure that additional medications or treatments do not conflict with the protocol. Also, most clinical trials offer short-term treatments for a certain illness or condition, but do not provide long-term or comprehensive primary health care.
What is informed consent?
Choosing to participate in a clinical research study is an important personal decision. Informed consent is just one part of a larger process designed to help safeguard people who are interested in participating in a clinical study.
Informed consent is the process of learning the key facts about a clinical study before deciding whether or not to participate. This process continues throughout the study as a way of providing information to participants.
What information does informed consent cover?
If you think you may be interested in participating in a clinical study, an informed consent document will be presented to you. This document includes detailed information about the study, including but not limited to the following:
- Objective or purpose of the study
- Study duration
- Required procedures
- Risks and potential benefits
- Key contacts
There are many other questions you may have or need to ask when you consider participation in a trial. We suggest that most questions be asked specific to the trial you are interested in joining. Some examples are below:
- What is the purpose of the study?
- What is the duration of the study?
- What tests and procedures are part of the study?
- How will my condition be monitored? What is the background of the principle investigators?
- Who are the staff involved involved in my care during the study?
- What are the risks involved?
- If the treatment works, can I continue to use the medication?
After reading through the document and discussing its contents with the study doctor or staff, it is up to you to decide if you want to sign the document and participate in the study. The informed consent document is not a contract – even if you sign the document, you are free to leave the study at any time.
Also, please see our Glossary of Terms to learn more about research.
Clinical Research Locations
-
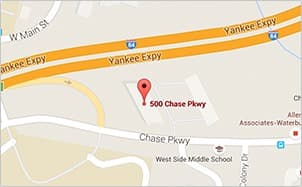
Waterbury Office
500 Chase Parkway, Waterbury, CT 06708 -
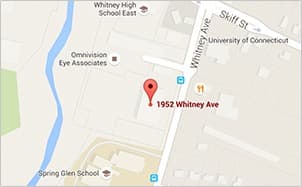
Hamden Office
1952 Whitney Avenue, Hamden, CT 06517
Contact Us